


Initiate multimodal pain management without delay (e.g., for confirmatory imaging).Identify associated injuries and complications that affect immediate management (e.g., open fracture, fracture-dislocation, neurovascular injury).Early reduction is vital to avoid vascular compromise and sciatic nerve injury. Posterior hip dislocations account for 90% of hip dislocations and typically follow a dashboard injury. Hip fractures can be associated with hip dislocation. Thromboembolism and osteonecrosis of the femoral head are common severe complications.
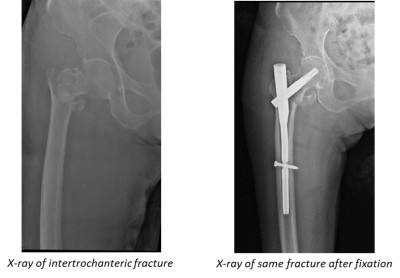
Older adults are at the highest risk of morbidity and mortality early involvement of geriatric care specialists is recommended for these patients. Nonoperative management may be considered for patients with severe comorbidities, although it is associated with a high mortality rate. Management typically includes multidisciplinary consultation, early pain management, IV fluid hydration, venous thromboembolism prophylaxis, and early surgical fixation. Comorbid conditions (e.g., anemia, acute kidney injury, delirium) are common with hip fractures. X-rays are usually diagnostic, but an MRI may be required to diagnose occult fractures or pathologic fractures. Clinical features include groin pain and deformity of the hip. Hip fractures in younger patients are usually caused by a high-energy impact (e.g., motor vehicle collision). Hip fractures in older adults are typically low-impact injuries and are often associated with osteoporosis. Hip fractures are classified as intracapsular (femoral head, femoral neck) or extracapsular (intertrochanteric, trochanteric, or subtrochanteric). Outcome studies indicate that conversion of Intertroch to THA is a less successful procedure, with higher rates of instability and greater troch pain, overall 88% survivorship at 10 years. Additionally, the fracture itself may have altered the anatomy of the proximal femur and thus increases the complexity of preparing the femur. The additional challenge of converting a failed Intertroch ORIF is an intertroch nonunion often requires a calcar replacing stem (about 65% of cases), and the stem must be long enough to bypass screw holes from the removed hardware which would otherwise act as stress risers. A screw and side plate is the preferred construct for the arthroplasty surgeon because removal can often be performed through the posterolateral approach used for the THA, and also because it preserves the abductor musculature. An intramedullary nail (hip IMN) is inserted through the abductor musculature and removal often causes further injury to the abductor complex, leading to postoperative limp and possible long term abductor deficiency and subsequent risk for instability. įailed Intertrochanteric Fracture ORIF (nonunion risk only 5%) is more complicated to revise. Outcomes suggest conversion failed femoral neck ORIF to THA is comparable to standard THA with 93% survivorship at 10 years (although possibly higher dislocation risk). Furthermore the femoral neck nonunion is excised with femoral preparation for the stem implant. Failed Femoral Neck ORIF (5-15% nonunion, 5-15% AVN) is often the easiest to convert to THA, as the standard treatment of 3 cannulated screws can be removed through the posterolateral incision for THA.


 0 kommentar(er)
0 kommentar(er)
